First, I will summarize some of the new strategies that are being developed for new and more effective treatments. Oxidative stress is an important target for treatment of ALS. Certainly, we already have one therapeutic agent, Radicava, that is aimed at scavenging the free radicals produced by oxidative stress that damage the cells. Investigators presented a different strategy—targeting the mechanisms that regulate the production of free radicals through the protective enzyme PDI, which acts to reduce the clumping (misfolding) of proteins and inhibit oxidative stress. Investigators have created novel molecules containing the active region of PDI and showed that these molecules were protective in cell and animal models.
Another strategy by Athira Pharma is examining the potential of small molecules modulating the neurotrophic hepatocyte growth factor system, which is neuroprotective and anti-inflammatory. One of these molecules, ATH1105, showed both independent and synergistic improvement in disease in a mouse model of ALS.
Another target discussed was the clumping of the protein TDP43, an important regulator of RNA processing to produce protein. TDP43 is found in the nucleus of cells in normal circumstances, but in ALS, it moves from the nucleus to the cell cytoplasm, where it clumps (aggregates), a finding in virtually all ALS neurons. It is hypothesized that the clumps may drive inflammation and degeneration. While there are trials designed to increase the clearance of these clumps, other strategies to reduce the amount of clumping are being developed.
One group of investigators showed that a small piece of a protein that regulates TDP43 improves function and survival in a fly model and mouse model of ALS. Other strategies are directed at ways to clear the clumped TDP43 through increases in a process called autophagy. These molecules showed improved survival in culture models. Other investigations focused on the loss of function that occurs when TDP43 moves out of the nucleus. Nuclear TDP43 is responsible for piecing together RNA properly to code for proteins. However, when it moves out of the nucleus, RNAs are not properly put together (this is called mis-splicing). The resultant proteins are not properly made and do not function as they should. Two important proteins that are affected by mis-splicing in ALS are UNC13 and STMN2. There are now genetic techniques being used to correct the RNA mis-splicing of STMN2 in trials, and we heard about a similar strategy to correct UNC13 RNA mis-splicing in cultured neurons. Finally, we heard about genetic strategies to alter the aggregates of small proteins that occur with the C9ORF72 expanded repeat, the most common genetic cause of ALS.
Of course, everyone is interested in the results of the clinical trials that were reported at the meetings. We heard some additional results from Valor, the trial of Tofersen (Qalsody) in SOD1 ALS. Qalsody is an antisense oligonucleotide that blocks the production of SOD1 and was recently approved by the FDA. Participants were allowed to continue the drug in an open label phase that has continued for up to 3 years. This has enabled additional observation of the efficacy. This data demonstrated a significant reduction in the neurofilament levels which reflects reduced neuronal degeneration as well as continued slowing of decline that continued over the period of analysis. Additionally, in a subset of participants there was an unexpected improvement in strength. Overall, there was improved survival, and for the rapid progressors, survival was extended by 1.6 years.
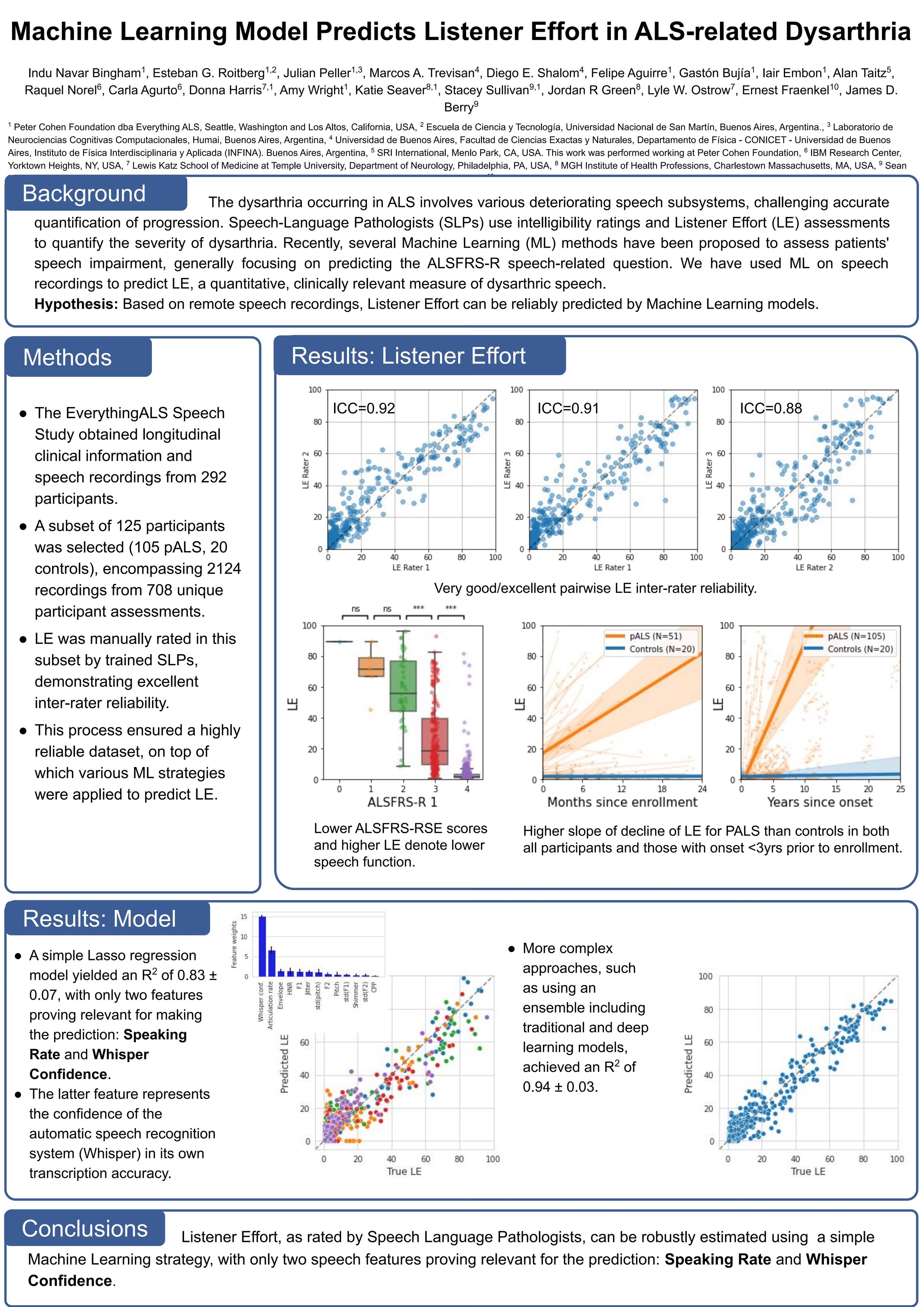
Promising results were reported on pridopidine, a small molecule that stimulates the Sigma 1 receptor and provides a neuroprotective effect. The phase 2 HEALEY ALS Platform Trial of pridopidine demonstrated it was safe and well tolerated. There were significant speech improvements compared to placebo, especially in speaking rate and articulation. Additionally, in the subgroup of participants with definite or probable ALS, early disease or fast progression, there were beneficial effects on measures of progression. This will help to design an upcoming Phase 3 trial.
Co-ALS, a phase 2 trial of colchicine (an already-approved drug that has an anti-inflammatory effect reduces clumping of proteins (TDP43) in cultures) demonstrated a decrease in the decline of function measured by the ALSFRS-R over 30 weeks, supporting further study of colchicine as a therapeutic agent. MIROCALS demonstrated a reduced risk of death when IL2, an anti-inflammatory molecule that drives T-regs (protective white blood cells), was administered with riluzole in a group of newly diagnosed ALS participants. Finally, we heard about apilimod dimesylate (AIT-101), which is directed at improving the clearance of clumped proteins including TDP43 through inhibition of an enzyme PIKfyve, which in turn causes the increase in a protein TFEB that increases the degradation of clumped proteins. This small trial in people with the C9ORF72 genetic variant of ALS demonstrated that AIT-101 was able to penetrate the brain and hit its target, with an increase in the activity of TFEB. This success will enable this molecule to move forward into Phase 2 in both sporadic and genetically-caused ALS.
While everyone has their focus on drugs that modify disease, we are learning more about the important role nutrition plays. Recently, I mentioned a paper that demonstrated omega 3 fatty acids could slow progression of ALS. At the meetings, a study of diet demonstrated that people living with ALS who consumed a diet that had a high glycemic index had slower disease progression and longer survival. The glycemic index reflects how much the sugar levels in your blood rise after eating a particular carbohydrate and is measured relative to pure glucose. Examples of high glycemic foods include white bread, rice, potatoes, and sugary soft drinks. This study underscores the need to maximize the interventions that are available now, including nutrition and respiratory support.